Historically, marketing campaigns promoting senior living have portrayed fun-loving communities, laden with activities like yoga and card games, with an overall positive morale. However, in reality, this is not the place that Canadians under the age of 75 want to be. In fact, this 2021 report revealed that 85% of all Canadians and 96% aged 65 or older said they would do anything to avoid moving into a long-term care home.
The reason is simple: most seniors under the age of 75 feel they’re still capable of living independently. They do not want to be moved away from their families, neighbours, and immediate communities where they’ve spent most of their lives.
Additionally, respondents feel that long-term care home staff are underpaid. Among respondents aged 65 years and older, 91% believe that Long-Term Care “LTC” homes are understaffed and 86% believe that staff are underpaid. The working conditions aren’t ideal, resulting in frequent staff shortages. Consequently, LTC home residents are unable to get the attention and/or care that they require, despite paying the high costs associated with living in such homes.
To address these challenges, several alternatives have been gaining prominence. One trend that’s getting traction internationally is establishing mixed-age communities with independent living for the seniors. These include residential communities and memory support communities, where the residents share kitchens and gardens. This way, the seniors that live within these communities have regular interactions with people, which reduces loneliness and fosters a positive environment. A similar initiative that’s already been launched in Canada is a home-sharing program. Canada HomeShare pairs a senior citizen with a younger individual, such as a college student. This benefits both parties as the college student can enjoy lower living costs, while the senior has someone who can help with tasks around the house. This solution offers the combined benefit of allowing seniors to age in place and have some social interaction at home.
The mixed-use project from Oxford Properties and Indi is of a viable option. This project is set to be completed in 2024. The community will boast a wide array of amenities and easy access to the central business district, in addition to public transit. It will also feature several public spaces where residents can meet and interact with each other, helping to create a close-knit community. One of the biggest benefits to senior residents will be the option to customise the housing units to their specific needs, allowing greater accessibility around the house and reducing the risk of injuries. risk of injuries.
A critical part of the solution to more innovative long-term care living environments is the increased use of technology. Given the prevalence of staff shortages, improved technology could help bridge that gap. Advanced tools that could benefit senior residents include things like motion sensors to alert staff when a resident falls, and voice command services to help seniors execute basic tasks around the house. This technology could be paired with telehealth offerings which would enable seniors to receive hospital care without leaving their home. This approach has already begun in some parts of Canada such as Alberton, Prince Edward Island where they started “A hospital without walls.” This initiative combines acute, primary, and geriatric care whereby, if successfully implemented, residents can access their healthcare from virtually anywhere.
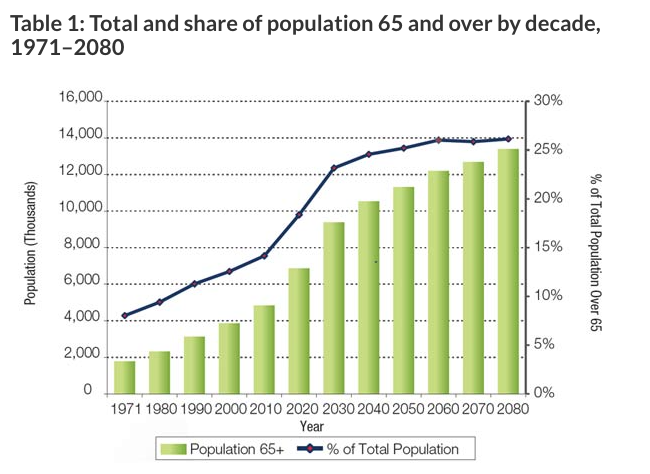
Solving this housing challenge may not seem urgent now, but it won’t be long before it is. The LTC system is a problem with a growing vector, based on the graph below. Eight years ago, Canadians over 65 represented 15.6 per cent of the population. By 2030, that number will increase to 23 per cent. This growth will certainly trouble the already overburdened LTC system if we don’t start pursuing more dignified solutions for our aging population now.
It’s clear to see there is a problem with Canada’s long-term care system, and innovation is required to solve it. These homes, that have always been known as the poor stepchild of the healthcare system, need more attention. Changes need to be made and they need to be employed in the best interests of the people that are most affected by it — our parents and grandparents.




